SAM & CMAM
What is SAM?
According to UNICEF, ‘Severe Acute Malnutrition (SAM) is the most extreme and visible form of undernutrition.’
SAM is a condition where the Weight for Height is -3 Standard Deviation. Children with this condition have very low weight for their height and severe muscle wasting. They may also have nutritional oedema – characterized by swollen feet, face and limbs. About two thirds of these children live in Asia and almost one third live in Africa.
Severe acute malnutrition is a major cause of death in children under 5, and its prevention and treatment are critical to child survival and development.
What are the causes of SAM?
- Poor access to appropriate, timely and affordable health care
- Inadequate caring and feeding practices, which includes lack of exclusive breastfeeding or low quantity and quality of complementary food
- Poor food security, which means an ongoing lack of food quantity and diversity, characterized in many resource-poor settings by a monotonous diet with low nutrient density, together with inadequate knowledge of patterns of food storage, preparation and consumption
- Low knowledge about food storage, preparation and consumption
- Lack of a sanitary environment, including access to safe water, sanitation and hygiene services
Prevention of SAM and Current State of SAM Treatment in India
Preventing SAM requires a comprehensive approach to address the diverse factors contributing to intergenerational malnutrition. Abject poverty, lack of employment, and regressive social practices, like poor girl child nutrition and early marriage, contribute to low birth weight and malnutrition. While initiatives like increasing the minimum age of marriage and family planning counseling are steps in the right direction, a more robust focus on nutrition is essential. The POSHAN Abhiyaan is a promising initiative, but studies indicate that current progress may not meet India’s nutrition targets or the 2030 UNICEF and WHO goals.
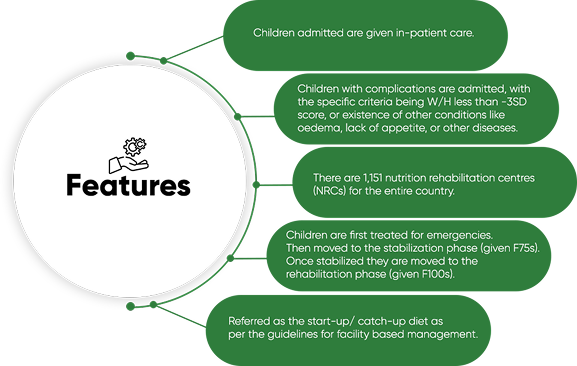
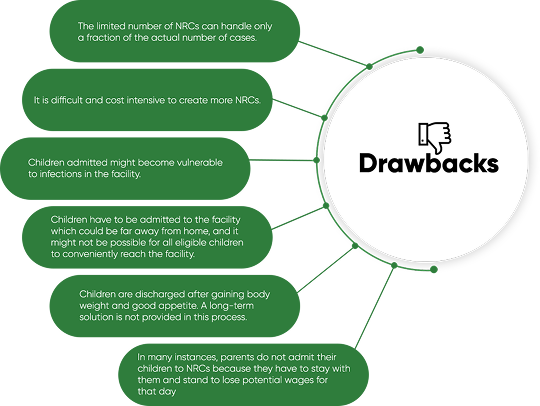
Currently, India’s primary SAM treatment strategy is facility-based care (F-SAM) at Nutritional Rehabilitation Centers (NRCs), catering to complicated cases. However, with limited NRCs, a vast majority of affected children remain underserved, as 90% of SAM cases do not require facility-based intervention.
This gap highlights the necessity of a community-based approach: Community-Based Management of Acute Malnutrition (CMAM). Recommended by UNICEF and WHO, CMAM is the standard protocol for uncomplicated SAM, which constitutes 85-90% of all cases. CMAM complements NRCs, creating a more comprehensive system.
The Need for a Community-Based Approach: CMAM
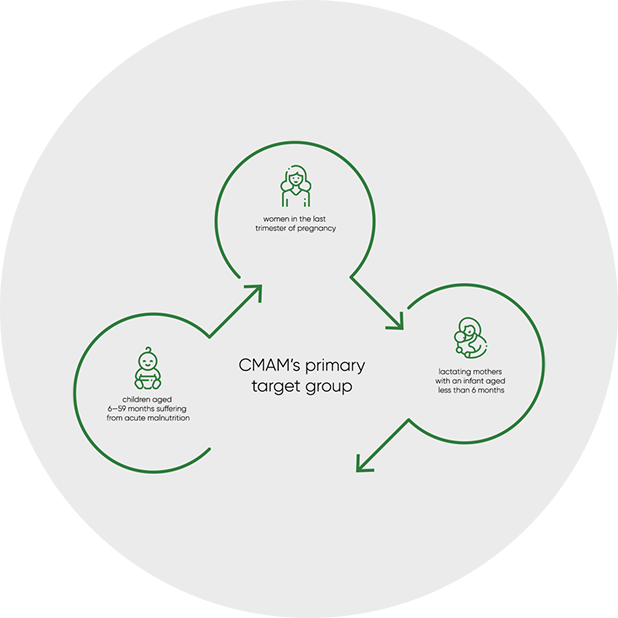
This gap highlights the critical need for a community-based strategy, namely the Community-Based Management of Acute Malnutrition (CMAM). Recommended by both UNICEF and WHO, CMAM is the standard treatment protocol for uncomplicated SAM, which accounts for approximately 85-90% of all cases. It’s crucial to understand that CMAM is not a replacement for NRCs, but rather a complementary approach designed to create a more comprehensive and effective system.
Key Advantages and Components of CMAM
CMAM focuses on managing uncomplicated SAM cases within the community, leveraging existing resources. This approach offers several key advantages:
- Infrastructure Efficiency: It can be implemented through the existing network of Anganwadis under the Integrated Child Development Services (ICDS) system, eliminating the need for new infrastructure.
- Cost-Effectiveness: It strengthens the existing community-based framework, making it cost-effective.
- Community Engagement: It proposes an in-built response mechanism through frontline health workers and mothers.
- Continuity of Care: It ensures continuity of care after discharge.
- Reduced Infection Risk: It reduces exposure to hospital-acquired infections.
CMAM is by no means a replacement of NRCs, but a fortification of the existing process that can eventually result in covering the maximum number of affected children.
Central to CMAM is the use of Ready-to-Use Therapeutic Food (RUTF), an emergency nutritional supplement provided for 8-12 weeks. Caregivers are also trained on proper nutritional habits, hygiene, and breastfeeding practices. Additionally, medications are provided to address common illnesses like diarrhea and edema, often associated with SAM. RUTF is a temporary intervention and does not interfere with the long-term dietary preferences of the child.
According to UNICEF, ‘Every US$ 1 invested in nutrition, including the treatment of severe acute malnutrition, generates as much as US$ 138 in better health and increased productivity. At the other end of the scale – not investing in nutrition perpetuates economic losses both to individuals and to countries – at an estimated cost of up to 11% of annual gross domestic product in lost productivity.
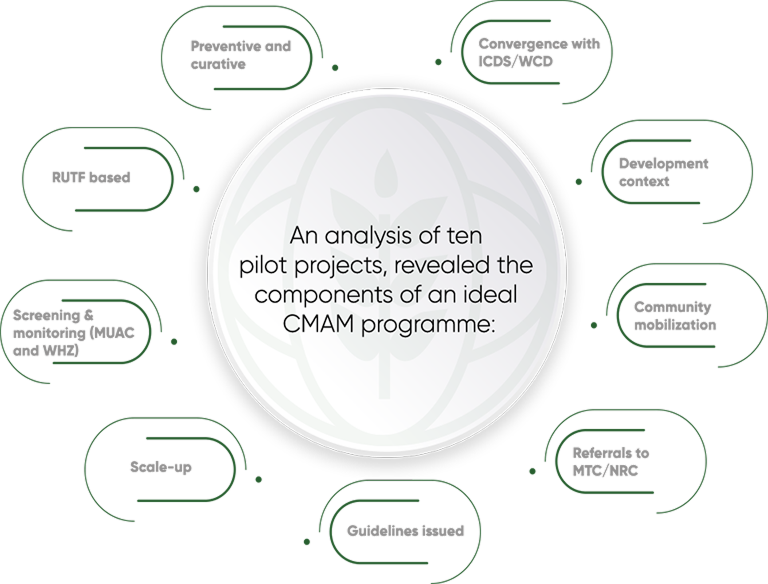
Evidence of CMAM’s Effectiveness
The effectiveness of CMAM has been demonstrated in various countries across Africa and Asia, as well as in pilot projects within Indian states like Rajasthan, Gujarat, Bihar, Madhya Pradesh, and Jharkhand. Notably, in Rajasthan, the state POSHAN program, utilizing RUTF, achieved a 70.4% recovery rate and reduced the mortality rate to 0.1%. This evidence underscores the potential of CMAM to significantly improve the treatment of SAM in India.