Community-based Management of Acute Malnutrition (CMAM) approach is widely recognized for its effectiveness in treating Moderate Acute Malnutrition (MAM) and Severe Acute Malnutrition (SAM) in children under 5 years. Found potent across different socio-economic and geographical settings, CMAM helps volunteers in identifying the target population and initiating treatment for children with acute malnutrition before they fall seriously ill and require medical attention. This approach assumes importance in the backdrop of a facility-based model having limited scope in terms of coverage and impact. CMAM comes in handy especially if there are aggravating factors present in the community such as epidemics, high death rate, food insecurity and a general lack of health infrastructure. Multiple pieces of evidence suggest that children with uncomplicated SAM can be treated effectively in their community setup without being admitted to a health facility.
Ready to Use Therapeutic Foods (RUTF) or locally prepared nutrient-dense foods serve as an indispensable component to treat SAM-afflicted children in their community environs and facilitate earlier recognition of SAM and the timely onset of treatment. In the case of uncomplicated SAM, a strong community component could go a long way in ensuring appropriate care through sensitization and mobilization. A skilled health worker facilitates the community in providing oral medication, RUTF and monitors the health parameters of children closely. A major public health impact is evident through greater reach and reduced mortality rate when applied at an appropriate scale. RUTF, containing high energy content, an adequate amount of vitamins and minerals can be consumed easily by children without adding water. They don’t require refrigeration and can be used even where hygiene conditions are not optimal. Research suggests that in a CMAM setup, regular and standardized doses of RUTF is the single most contributing factor in eliminating SAM in children, especially those living in unhygienic, risk-prone regions without access to nutritious food.
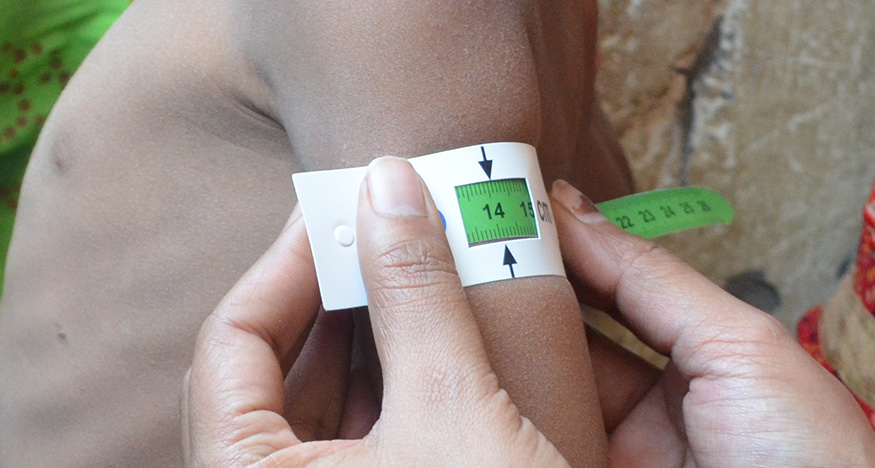
CMAM approach’s ingenuity lies in dealing with both complicated and uncomplicated cases effectively, catering to both spectrums of SAM. Regular screening by volunteers enables the early detection and treatment of malnutrition. In the case of medical complications, children are referred to as inpatient care facilities for intensive treatment. When their health stabilizes, they are referred back to a decentralized community care facility. The components of CMAM include community-based mobilization regarding best practices, screening of children to prioritize treatment vectors, continuous counselling and education regarding RUTF nutrition, and regular follow-ups and monitoring of child’s health. CMAM stands to gain by establishing linkages with other complementary programs and tapping into their logistics and benefits.
Shorter recovery periods for children (usually <4 weeks), proven effectiveness during humanitarian emergencies, reduced chances of cross-infection, higher coverage of services, lower Out of Pocket Expenses (OOP) and empowered community capacity make CMAM a strong alternative compared to traditional in-patient care which is resource-intensive. UN prescribes CMAM as a standard care methodology for curing acute malnutrition. Low mortality and high cure rates among non-defaulting children usually characterize CMAM implementations, especially in poor nations. When properly integrated with other long-term health interventions, CMAM could go a long way in developing a healthy human capital and achieving mainstream food security sustainably and cost-effectively.
References
- https://www.wvi.org/nutrition/project-models/cmam
- https://www.who.int/nutrition/topics/Statement_community_based_man_sev_acute_mal_eng.pdf
- https://www.usaid.gov/global-health/health-areas/nutrition/technical-areas/community-based-management-acute-malnutrition
- https://www.ncbi.nlm.nih.gov/pubmed/25833981